Case 1.: Thromboembolic side effect of the chemotherapy treatment of a progressive tumor
A 50-year-old female patient palpated a 1.5-2 cm lesion in the inner upper quadrant of the right breast. Mammography revealed tiny calcifications in the right breast, on the border of the outer quadrants, 7 cm from the mamilla. After an excision on the right breast, regarding that a non-palpable lesion also contained breast carcinoma, mastectomy and ABD was carried out in November 2002 at the SZTE Department of Surgery. IDC, Grade III, pT1 (15 mm), pN0, ER 80%, PR 90 % positive, C-erB-2:++, HER2 FISH: an IDC (Grade III, pT1 (15 mm), pN0, ER 80%, PR 90 % positive, C-erB-2: ++, HER2 FISH negative), as well as DCIS. The patient received 6 cycles of adjuvant CEF treatment after surgery and adjuvant hormone treatment (tamoxifen) for 5 years. In November 2008 the patient underwent pleurodesis due to hydrothorax. Chest CT showed lymph node metastases. Abdominal CT and bone scan were negative. In January 2009, we started her paclitaxel-bevacizumab treatment within a clinical trial. After 15 treatments (5 cycles) severe dyspnea has been reported.
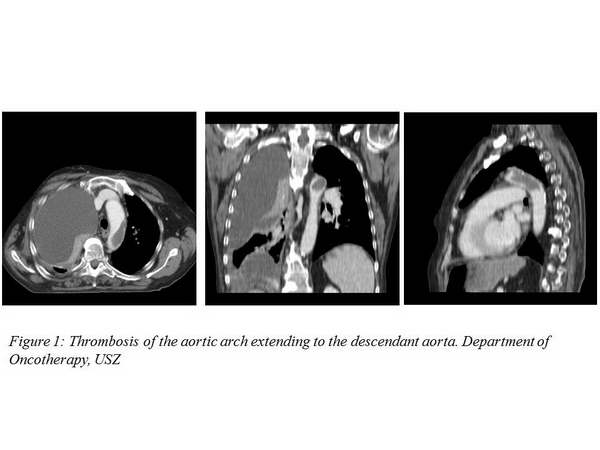
Chest CT showed a contrast material filling defect 3 cm in diameter in the aortic arch that corresponded to a thrombus (Figure 1.).
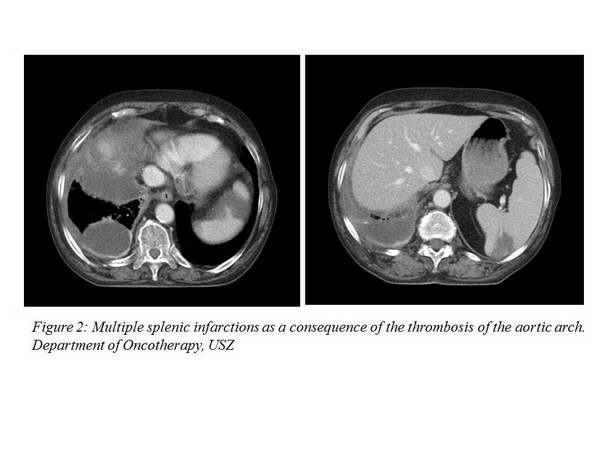
As a result of the aortic thrombus, splenic infarctions developed (Figure 2.).
In addition, a right hydrothorax has developed repeatedly (Figure 3.).
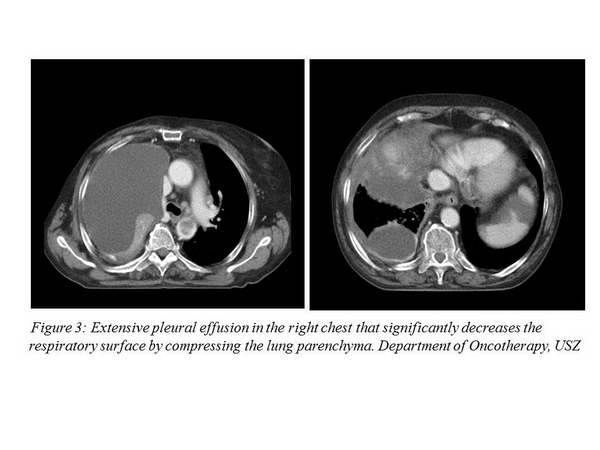
The patient received anticoagulant treatment, and chest drainage was performed with pleurodesis. Following that, the patient’s condition has gradually progressed and in August 2009, she died of respiratory failure.
Edited by Dr. Ágnes Dobi









